A stroke is caused by blockage of an artery or blood vessel preventing blood from getting to your brain cells. This blockage causes 1.9 million brain cells to die every minute. No age group is immune from a stroke. Even infants can have a stroke.
If not treated immediately, stroke will, among other things, affect your ability to speak, your ability to walk, and even to feed yourself. In general, you will not be able to take care of yourself. Getting immediate help can reduce the severity of these effects. Recovery can take a lifetime.
You can tell if a person is having a stroke by using the acronym
F.A.S.T.
to recognize the following symptoms:
F. (Face) - Does one side of their face droop?
A. (Arms) - If they hold their arms straight out in front of them, with eyes closed, does one arm slowly drift down?
S. (Speech) - When you ask them to repeat a simple sentence like, "Mary had a little lamb.", is their speech slurred or sound strange?
T. (Time) - Call 911 immediately!
Other symptoms are: trouble seeing in one or both eyes, confusion, severe headache, loss of balance and inability to move on one side of the body.
Calling 911 is essential because time is critical, and the Emergency Medical Technicians can do a preliminary diagnosis and get a stroke team standing by while they are en-route to the hospital. You have a very limited time to get effective treatment and much of this time is spent in diagnosing the severity and type of your stroke.
Certain types of stroke, such as Ischemic, can be effectively treated with a clot busting drug called t-PA. It is an FDA approved drug researched and developed by GENENTECH.
t-PA must be administered within three hours of the onset of stroke symptoms to be effective.
You can reduce your chances of having a stroke. Know your risk factors. They include: high blood pressure, high cholesterol, diabetes, smoking and low physical activity.
Remember
F.A.S.T.
Face. Arms. Speech. Time.
---
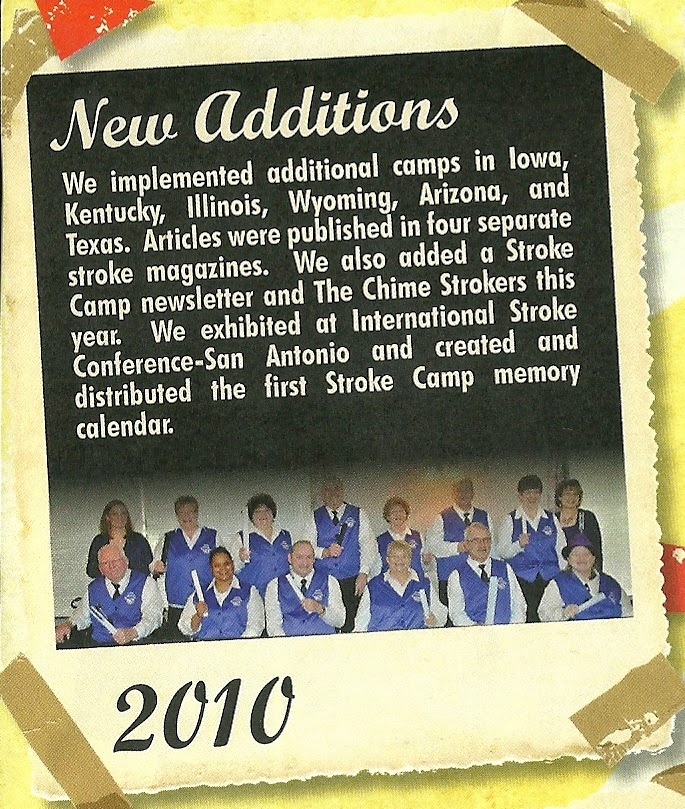
Here is a screen shot from our Retreat & Refresh Stroke Camp Learning Center that we use to promote stroke awareness.